Overview
Diabetes is a chronic health condition that affects millions globally. It occurs when the body either doesn’t produce enough insulin or can’t use insulin effectively. This leads to elevated blood sugar levels, which, if left unmanaged, can result in serious complications like heart disease, kidney failure, nerve damage, and vision loss.
Effective Diabetes Management focuses on regulating blood glucose levels through lifestyle changes, medication, and regular monitoring. The condition requires a personalized care plan that includes nutrition, physical activity, and stress management.
The three primary types of diabetes are:
- Type 1 Diabetes: An autoimmune condition where the pancreas stops producing insulin. It typically develops in children and young adults.
- Type 2 Diabetes: The most common form, usually developing in adults due to lifestyle factors and genetics. It can often be prevented or delayed with healthy habits.
- Gestational Diabetes: A temporary condition during pregnancy that can increase the risk of Type 2 diabetes later in life.
Early diagnosis, consistent follow-up, and a strong support system are crucial to successful Diabetes Management.
Symptoms
Recognizing the symptoms of diabetes early can lead to timely diagnosis and better Diabetes Management. While symptoms may vary based on the type and severity, common signs include:
- Frequent urination, especially at night
- Excessive thirst and dry mouth
- Persistent fatigue or weakness
- Unexplained weight loss despite regular eating
- Slow-healing cuts and wounds
- Frequent infections (skin, urinary, gum)
- Blurred or reduced vision
- Tingling or numbness in hands and feet
- Increased hunger after meals
If you or a loved one experiences any of these signs, consult a healthcare provider for screening and diagnosis. Early intervention greatly improves long-term outcomes.
Precautions
Prevention is a vital aspect of Diabetes Management. Taking the right precautions can reduce your risk of complications and improve quality of life.
- Maintain a healthy weight and body mass index (BMI)
- Consume a balanced diet rich in fiber, vegetables, lean proteins, and whole grains
- Limit refined sugars and processed carbohydrates
- Engage in at least 150 minutes of moderate exercise per week
- Quit smoking and limit alcohol intake
- Get routine health screenings, including eye exams and foot checks
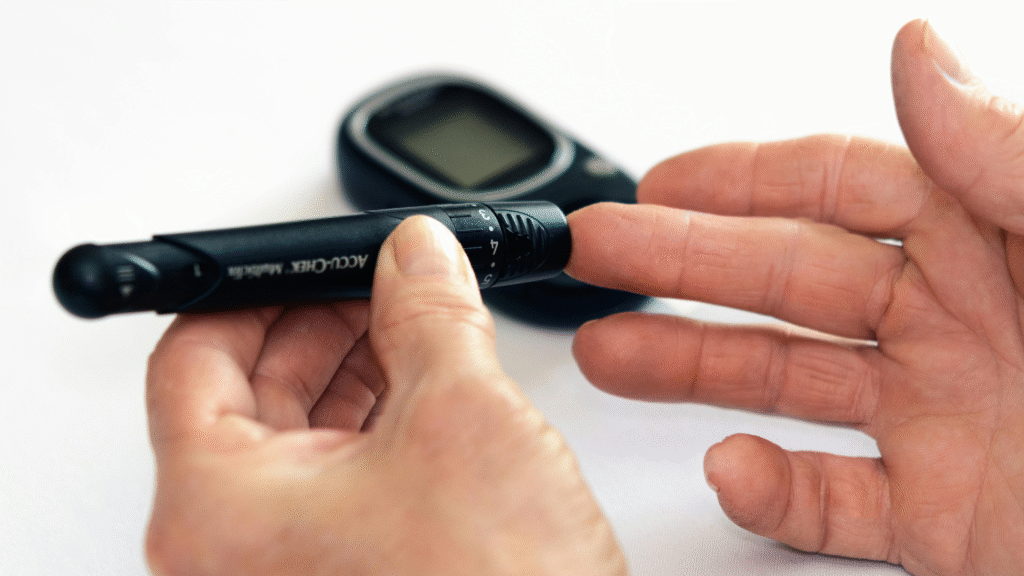
- Monitor blood sugar levels as advised by your doctor
- Learn about your condition and stay informed
Even small, consistent lifestyle changes can lead to major improvements in diabetes prevention and control.
Solutions
Managing diabetes effectively requires a holistic approach. The following solutions are key pillars of long-term Diabetes Management:
- Personalized Meal Planning: A diabetes-friendly diet helps keep glucose levels stable and supports weight control.
- Daily Physical Activity: Exercise improves insulin sensitivity, blood circulation, and energy levels.
- Monitoring Blood Glucose: Regular checks help you respond quickly to highs and lows and adjust your plan accordingly.
- Medications & Insulin: Depending on the type and progression of diabetes, treatment may include oral drugs or insulin injections.
- Stress Reduction: Chronic stress can spike blood sugar. Mindfulness, meditation, and hobbies can be effective tools.
- Sleep Hygiene: Poor sleep is linked to insulin resistance. Aim for 7–9 hours of quality sleep nightly.
Diet Recommendations
Diet plays a central role in Diabetes Management. A well-structured eating plan can help stabilize blood glucose, reduce insulin resistance, and maintain energy levels throughout the day.
Foods to Include:
- Whole grains like quinoa, oats, barley, and brown rice
- Non-starchy vegetables such as spinach, broccoli, kale, and zucchini
- Lean proteins like fish, turkey, eggs, and legumes
- Healthy fats from avocado, olive oil, and nuts
- Fruits in moderation, especially berries, apples, and citrus
Foods to Limit or Avoid:
- Sugary beverages like soda, energy drinks, and sweetened juices
- Refined carbs such as white bread, pastries, and candy
- Fried and processed foods
- Excessive salt and high-fat dairy
Consult a registered dietitian for a personalized meal plan tailored to your lifestyle, cultural preferences, and diabetes type.
Lifestyle Tips for Managing Diabetes
Adopting the right lifestyle choices plays a pivotal role in Diabetes Management. Lifestyle modifications can help control blood glucose, prevent complications, and improve overall well-being. Here are key lifestyle habits to incorporate:
1. Regular Physical Activity
Exercise helps your body use insulin more effectively and lowers blood sugar. Aim for at least 150 minutes of moderate aerobic exercise each week, along with muscle-strengthening activities. Activities like walking, swimming, and cycling are excellent options.
2. Stress Management
Stress can raise blood sugar levels. Finding ways to manage stress, such as through yoga, meditation, deep breathing exercises, or hobbies, can help keep glucose levels under control.
3. Quality Sleep
Adequate sleep is essential for optimal diabetes control. Aim for 7 to 9 hours of sleep each night. Poor sleep can increase insulin resistance, making it harder to manage diabetes effectively.
4. Stay Hydrated
Drinking plenty of water helps prevent dehydration and supports kidney health, which is especially important for those with diabetes. Avoid sugary drinks that can cause blood sugar spikes.
5. Avoid Smoking
Smoking worsens circulation and increases the risk of diabetes-related complications such as heart disease. Quitting smoking significantly improves overall health and helps manage diabetes better.
Making these lifestyle adjustments can greatly improve blood sugar control and enhance your quality of life. The key is consistency and making gradual, sustainable changes that work for you.
When to See a Doctor for Diabetes
If you have diabetes or suspect you may have it, seeing a healthcare provider regularly is crucial for managing your condition and preventing complications. Here are situations when you should contact your doctor:
1. If You Notice Unexplained Symptoms
If you’re experiencing symptoms like excessive thirst, frequent urination, blurred vision, unexplained weight loss, or fatigue, it’s essential to consult a doctor for a blood test to check your glucose levels.
2. If Your Blood Sugar Is Hard to Control
If you’re struggling to keep your blood sugar levels in range despite following your treatment plan, adjustments to your medication, diet, or exercise plan may be necessary. A healthcare professional can help tailor a solution.
3. If You Develop Complications
Diabetes can cause complications such as nerve damage, kidney disease, heart problems, and eye issues. If you notice tingling, numbness, poor circulation, or difficulty seeing clearly, make an appointment immediately.
4. If You’re Pregnant and Develop Gestational Diabetes
Gestational diabetes is diagnosed during pregnancy and requires careful monitoring. After giving birth, women with gestational diabetes should follow up with their doctor to monitor for potential development of Type 2 diabetes later in life.
5. Annual Check-ups and Preventive Care
Regular check-ups are essential for maintaining diabetes management. Your doctor will help monitor your blood sugar, A1C levels, kidney function, eye health, and nerve health. These assessments are critical to catching early signs of complications.
Remember, proactive care is the best way to manage diabetes and prevent complications. Stay connected with your healthcare team and follow their advice to live a healthier, more balanced life.
Prevention of Diabetes
While Type 1 diabetes cannot be prevented, Type 2 diabetes is largely preventable through lifestyle changes. If you are at risk of developing Type 2 diabetes, making the following changes can significantly lower your chances:
1. Maintain a Healthy Weight
Being overweight is a major risk factor for Type 2 diabetes. Losing even 5–10% of your body weight can improve insulin sensitivity and reduce the risk of developing diabetes.
2. Stay Physically Active
Regular physical activity helps improve insulin function, control blood sugar levels, and maintain a healthy weight. Aim for at least 30 minutes of exercise per day, 5 days a week.
3. Eat a Balanced Diet
Eating a diet rich in fruits, vegetables, whole grains, and lean proteins can help maintain healthy blood sugar levels. Avoid sugary foods, refined carbs, and high-fat processed foods.
4. Monitor Blood Sugar Levels
If you are at risk for diabetes or prediabetes, it’s important to monitor your blood sugar levels regularly. Early detection allows for early intervention, including changes in diet and lifestyle.
5. Avoid Smoking and Limit Alcohol
Smoking increases the risk of diabetes complications, while excessive alcohol consumption can disrupt blood sugar control. Avoid smoking and limit alcohol intake to lower your risk.
Making these preventive steps a part of your daily life can significantly reduce your risk of developing Type 2 diabetes. Start small and stay consistent for the best results.
Frequently Asked Questions (FAQs)
- Can diabetes be cured? – Currently, there is no cure for diabetes, but it can be managed with lifestyle changes, medication, and insulin therapy.
- Is Type 1 diabetes more serious than Type 2? – Type 1 diabetes requires lifelong insulin therapy, while Type 2 can often be managed with diet and exercise, but both require serious management to prevent complications.
- Can I eat sugar if I have diabetes? – Yes, but in moderation. You should monitor your blood sugar levels after consuming sugary foods to ensure they stay within the recommended range.
- What are the long-term effects of poorly managed diabetes? – Long-term complications of uncontrolled diabetes can include cardiovascular disease, kidney failure, nerve damage, and vision problems.
- How often should I check my blood sugar? – The frequency of blood sugar checks depends on the type of diabetes and your treatment plan. Discuss with your doctor for a personalized schedule.
For more information on managing diabetes, it’s always a good idea to consult with your healthcare provider for tailored advice and treatment options.
Causes
The causes of diabetes vary based on the type of the disease. Understanding these causes is crucial in both preventing and managing diabetes effectively. Below, we delve into the factors that contribute to the development of diabetes.
1. Genetics and Family History
Diabetes often runs in families. Family history is a significant risk factor for both Type 1 and Type 2 diabetes. If you have close relatives, such as a parent or sibling, with diabetes, your chances of developing the condition increase. This is especially true for Type 2 diabetes, where genetics plays a major role. For Type 1 diabetes, genetic predisposition may make the immune system more likely to attack the insulin-producing cells of the pancreas, though environmental factors (such as viral infections) may trigger the disease. Understanding family medical history helps in assessing personal risk and initiating early preventive measures.
2. Autoimmune Attack (Type 1)
Type 1 diabetes is an autoimmune disorder in which the body’s immune system mistakenly attacks and destroys the beta cells in the pancreas that are responsible for producing insulin. Without insulin, the body cannot regulate blood sugar, which leads to high glucose levels in the bloodstream. This form of diabetes is typically diagnosed in children or young adults, although it can occur at any age. The exact cause of this autoimmune response remains unclear, but scientists believe that environmental triggers, such as viruses, may play a role in initiating the immune system’s attack. Genetic factors also contribute to susceptibility, though it is not a hereditary disease in a direct sense. Currently, there is no known cure, but Type 1 diabetes is managed through daily insulin therapy.
3. Obesity and Sedentary Lifestyle (Type 2)
Obesity is the most significant risk factor for Type 2 diabetes. When the body accumulates excessive fat, especially in the abdominal area, it leads to insulin resistance. Insulin resistance means that the body’s cells no longer respond to insulin as effectively, resulting in higher blood sugar levels. Over time, the pancreas produces more insulin to compensate, but eventually, it cannot keep up, leading to Type 2 diabetes. Obesity promotes inflammation and hormonal imbalances that make it even harder for the body to regulate glucose. A sedentary lifestyle, characterized by minimal physical activity, worsens insulin resistance. Regular physical activity can help improve insulin sensitivity, and even a modest weight loss can significantly reduce the risk of developing Type 2 diabetes.
4. Insulin Resistance
Insulin resistance is a key factor in the development of Type 2 diabetes. Normally, insulin helps cells absorb glucose from the bloodstream for energy or storage. In insulin resistance, the body’s cells (particularly muscle, fat, and liver cells) become less responsive to insulin, meaning that glucose cannot enter the cells as effectively. To compensate for this, the pancreas increases insulin production, but over time, the pancreas can’t keep up with the demand, leading to elevated blood sugar levels. Insulin resistance often develops due to obesity, especially excess fat in the abdominal area, and is also exacerbated by a lack of physical activity. Insulin resistance is a progressive condition and can go unnoticed for years, as symptoms may be subtle or absent. However, it increases the risk of developing Type 2 diabetes and other metabolic conditions, such as cardiovascular disease.
5. Hormonal Changes During Pregnancy (Gestational Diabetes)
Gestational diabetes occurs during pregnancy and is marked by high blood sugar levels that develop due to hormonal changes. During pregnancy, the placenta produces hormones that make the body less responsive to insulin, a phenomenon known as insulin resistance. As the pregnancy progresses, the body may struggle to produce enough insulin to overcome this resistance, resulting in elevated blood sugar. Gestational diabetes affects about 2-10% of pregnancies and usually resolves after childbirth. However, women who experience gestational diabetes are at a higher risk of developing Type 2 diabetes later in life. Babies born to mothers with gestational diabetes are also at risk of health issues, including being overweight at birth, having low blood sugar levels at birth, and developing obesity and Type 2 diabetes later in life.
6. Age
As you age, your risk for developing Type 2 diabetes increases. This is partly due to changes in insulin sensitivity and a tendency to gain weight as metabolism slows down. Older adults are more likely to have other risk factors for diabetes, such as high blood pressure, high cholesterol, and reduced physical activity, which all contribute to insulin resistance. People over the age of 45 are more likely to develop Type 2 diabetes, and the risk continues to rise as age increases. Regular health checks and lifestyle changes can help mitigate these risks as you get older.
7. Ethnicity
Certain ethnic groups have a higher risk of developing Type 2 diabetes due to a combination of genetic and environmental factors. These groups include African American, Hispanic, Native American, Asian American, and Pacific Islander populations. The reasons behind this increased risk are not fully understood, but it is believed that genetic predisposition, lifestyle factors, and diet play a role. For example, individuals in these groups may have a higher tendency to develop insulin resistance, obesity, or metabolic syndrome, all of which increase the risk of Type 2 diabetes. Awareness of these factors can help in early detection and prevention within at-risk communities.
8. High Blood Pressure (Hypertension)
High blood pressure, or hypertension, is closely associated with diabetes, particularly Type 2 diabetes. Having high blood pressure can damage blood vessels and make it harder for insulin to do its job of controlling blood sugar. Additionally, hypertension is often part of a condition called metabolic syndrome, which includes obesity, high cholesterol, and insulin resistance, all of which increase the risk of Type 2 diabetes. Managing blood pressure through lifestyle changes, diet, and medications can help reduce the risk of developing diabetes and prevent complications in those who already have the condition.
9. Polycystic Ovary Syndrome (PCOS)
Women with Polycystic Ovary Syndrome (PCOS) are at an increased risk of developing Type 2 diabetes. PCOS is a hormonal disorder that causes insulin resistance, leading to higher blood sugar levels. The condition also causes irregular menstrual cycles, excess androgen (male hormones), and enlarged ovaries with cysts. Insulin resistance in women with PCOS is common and can lead to Type 2 diabetes if not managed. Managing PCOS with lifestyle changes, weight control, and medications can help prevent the progression to diabetes.
10. Other Medical Conditions
Certain other health conditions can increase the risk of developing diabetes, including:
- High Cholesterol: Elevated cholesterol levels are often linked to insulin resistance and Type 2 diabetes.
- Sleep Apnea: People with obstructive sleep apnea are more likely to develop Type 2 diabetes due to disrupted sleep patterns and hormonal imbalances.
- Chronic Inflammation: Persistent low-level inflammation in the body can contribute to the development of insulin resistance.
More Diabetes Management Blogs From Other Sources
Diabetes Management – Symptoms and causes
Diabetes Management: What It Is, Causes, Symptoms, Treatment & Types
Everything You Need to Know About Diabetes Management
Diabetes Management- Medical Encyclopedia
✅ Visit SearchYourFitness.com For More Blogs
CLICK HERE TO READ US ON QUORA
YOUR NEEDS 😉
Click any tool below to explore and calculate instantly!